
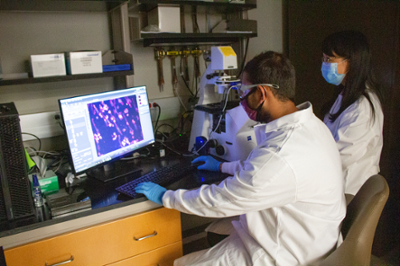
Dr. Feng Zhao, associate professor in the Department of Biomedical Engineering at Texas A&M University, is innovating ways we treat tissue damage in the body.
Zhao’s expertise is in cardiovascular tissue engineering and tissue vascularization (where a capillary network capable of delivering nutrients to the cells is formed within the tissue). Applications range from cardiac patches and vascular grafts for bypass surgeries to wound healing.
To ensure an engineered tissue is accepted by the body, a common strategy is to start the process of building the 3D structure of a material that mimics the natural tissue as much as possible, including using tools to organize the cells into a tissue structure so that the engineered tissues can be better integrated into the body.
“You want to mimic a natural process because the cells can better perform their function in an environment that they are familiar with,” Zhao said. “It's not that easy to fully replicate the in vivo environment, but we try to do that.”
One tissue engineering challenge is ensuring the graft is vascularized and nourished, similar to the natural tissue. Through vascular bioengineering, Zhao said researchers could work to ensure that engineered 3D tissues contain the vessels and capillaries necessary for vascularization when the structure or scaffold is placed in the patient.
One of her newer projects focuses on lymphatic tissue regeneration to limit the chance of lymphedema — the build-up of fluid in soft body tissues when the lymph system is damaged or blocked — after cancer surgeries. Lymphatic tissue vessels remove extra fluid, but if the tissue is damaged after a trauma like surgery, Zhao said lymphedema could easily develop as the fluid cannot be removed.
“We have developed some tools to engineer the lymphatic microvessels in vitro that highly mimic the in vivo process of the lymphatic microvascular formation,” Zhao said. “However, it’s still not enough to fully restore the function of lymphatic tissue.
Unlike other tissues, lymphatic tissue contains capillaries and vessels of varying sizes, and larger vessels contain valves that ensure the unidirectional flow of collected fluids. Since Zhao’s model has shown success, her team is now working on developing models for larger and valved vessels.
“We are still striving to seek a perfect solution,” Zhao said. “We are tissue engineers. We use our unique way to recover the damaged tissue to its original shape and function.”
