
For decades, biomedical engineers have used their acumen to revolutionize healthcare through the development of devices, tools, equipment, techniques, and pharmaceuticals that have advanced the medical field in ways previously unimaginable.
While patients around the world have benefited from this ingenuity, those patients almost exclusively have had one thing in common-they’ve all been human.
Researchers in the Texas A&M College of Veterinary Medicine & Biomedical Sciences (CVM) and the Texas A&M College of Engineering have teamed up to begin filling that gap in the biomedical engineering field--that of veterinary medicine-by exploring the possibilities of what can be accomplished when innovative minds come together.
Getting to the Heart of the Problem
Dr. Ashley Saunders, a professor of cardiology and clinician in the Veterinary Medical Teaching Hospital’s (VMTH) small animal cardiology service, began using 3D imaging and printing to create models of the heart to aid in the teaching of anatomy and preparing for complex surgeries for animals. But while 3D models are useful in this regard, the technology has not been a definitive training tool, especially in the case of treating minimally invasive cardiology defects.
Cardiology residents are taught heart and blood vessel catheterization through observation and practice, relying on an understanding of the anatomy and the feel of inserting a catheter to perform a procedure.
Teaching catheterization using 3D printed models is difficult because doctors can’t see inside the blood vessels they’re trying to navigate, and it’s also difficult to replicate the feel of an animal’s blood vessels; therefore, doctors have to learn catheterization on a beating heart.
"That’s how you learn." Saunders said. "That’s how I learned."
Because heart defects like patent ductus arteriosus (PDA)--a congenital defect characterized by an opening between two blood vessels leading from the heart--are the most commonly addressed congenital defect by cardiologists at Texas A&M’s Small Animal Hospital (SAH), Saunders began looking to create a safer environment in which residents could learn and practice, one in which the stakes weren’t quite so high.
Enter Dr. Duncan Maitland, the Stewart & Stevenson Professor I in the College of Engineering’s Department of Biomedical Engineering, and Dr. Mark Wierzbicki, a postdoctoral researcher in Maitland’s Biomedical Device Laboratory.
Synthesizing a Solution
Maitland, whose research focuses on novel treatments for cardiovascular disease, had previously worked with a VMTH cardiovascular doctor to create devices for use in the operating room; the doctor encouraged Maitland and the biomedical engineers in his lab to move toward creating devices for animal patients.
"I learned long ago that we could reduce the number of animal iterations on device development if we brought clinicians in, or even imported our models into the clinical environment for more advanced testing," Maitland said. "Just getting iterations on models of real anatomies reduces the number of animals that need to be used in studies, and the quality of devices goes up exponentially."
Maitland’s lab had developed blocks made of silicone to test devices created to treat cardiovascular diseases. One day, Saunders toured Maitland’s lab and immediately began thinking about how the technology could be applied to help her train residents to treat PDA.
"The silicone block was made to resemble a PDA, and I knew we could use the 3D prints from our patients to make one that is more anatomically correct," Saunders said.
And that’s exactly what she and Wierzbicki, a doctoral student at the time, did. The two put their heads together and devised a plan that would combine the 3D imaging technology Saunders was already using with the silicone-based technology Wierzbicki was exploring for his dissertation.
The final product looks like a clear, rubber block, inside which, upon closer inspection, has the outline of several "tubes." These tubes are arteries cast from the actual heart from one of Saunders’ canine patients. To make the cast, Saunders used CT scans to create a 3D representation of the dog’s heart printed on the 3D printer in Maitland’s laboratory.
"We were able to 3D print the CT scanned heart using a dissolvable material and vapor polish the printed model to smooth out the ridges from the 3D printing process," Wierzbicki said. "We took the smooth, 3D printed heart, cast silicone around the model, and then dissolved out the 3D-printed part. After completing those steps, we were left with a model Dr. Saunders could use for training."
The result was a solution to multiple problems--not only did the project become part of Wierzbicki’s dissertation, but it produced anatomically correct, customized models that might change the way budding cardiologists are trained to learn catheterization techniques and repair heart defects.
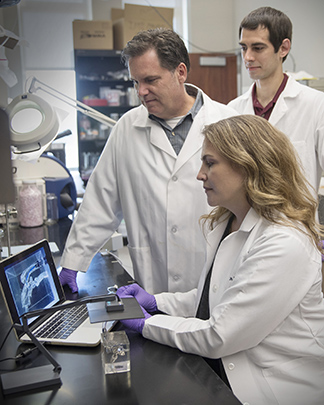
To create an even more realistic setting, Saunders incorporated a camera that projects what the doctors are seeing onto a computer screen so that they train on a simulated heart that mimics a true procedure.
"When we do these procedures in a dog, we can’t see inside the body; we use fluoroscopy, with images displayed on a screen that we have to look up at. So, it is important to learn how to do these procedures by watching a screen," she said. "We can mimic the procedure by having the silicone blocks, because they have the anatomy inside, and the block is clear, so they can see through it; the document camera displays the image up on my computer screen.
"They watch as they pass a catheter in and they learn how to do the procedure by getting the feel of inserting a device," she said. "It doesn’t require fluoroscopy or radiation, and it doesn’t require them being inside an actual dog to practice for the first time."
The best part--the silicone blocks are virtually indestructible.
"This means you can take the block into a training lab setting, knowing that it’s going to stand up to being used over and over again," Saunders said.
The future of biomedical engineering: Just a Heartbeat Away
Because of what the model means for how doctors treat cardiac defects, Saunders, Wierzbicki, and Maitland have published multiple papers related to the model and other devices used in cardiology.
Saunders also has begun using the model in training exercises and labs for both residents and specialists who have an interest in catheterization techniques and interventional cardiology. During a recent training that included specialists from around the world, Saunders found that the doctors responded enthusiastically to the model.
"They really loved it," she said. "They said they feel like they’re more comfortable practicing with the model, it makes more sense to them."
While most companies that manufacture devices for human cardiology currently aren’t interested in making devices for animals, as more and more veterinary surgeons begin recognizing the value of this kind of model, Maitland said he hopes that attention will open the doors for more opportunities for collaboration between biomedical engineers and the field of veterinary medicine.
"If you look at all of engineering, and biomedical engineering specifically, you don’t think about animal health care as a primary focus. We’re not trained to do that, and so there are not enough partnerships going on between the two colleges, and specifically biomedical and the CVM," said Maitland, who is chairing a committee in his department to do just that. "I think we could make a lot of impact, and in this case, not just with what Ashley is developing for training, but we can also impact the technologies that are used in animal health care significantly, if we just pay attention to it."
This article originally appeared in the Spring 2018 edition of CVM Today.
